A common question that people living with diabetes often ask is whether their condition can increase the development of glaucoma. This condition is a serious eye disorder that can lead to permanent vision loss, making it especially important for individuals with diabetes to understand the risks.
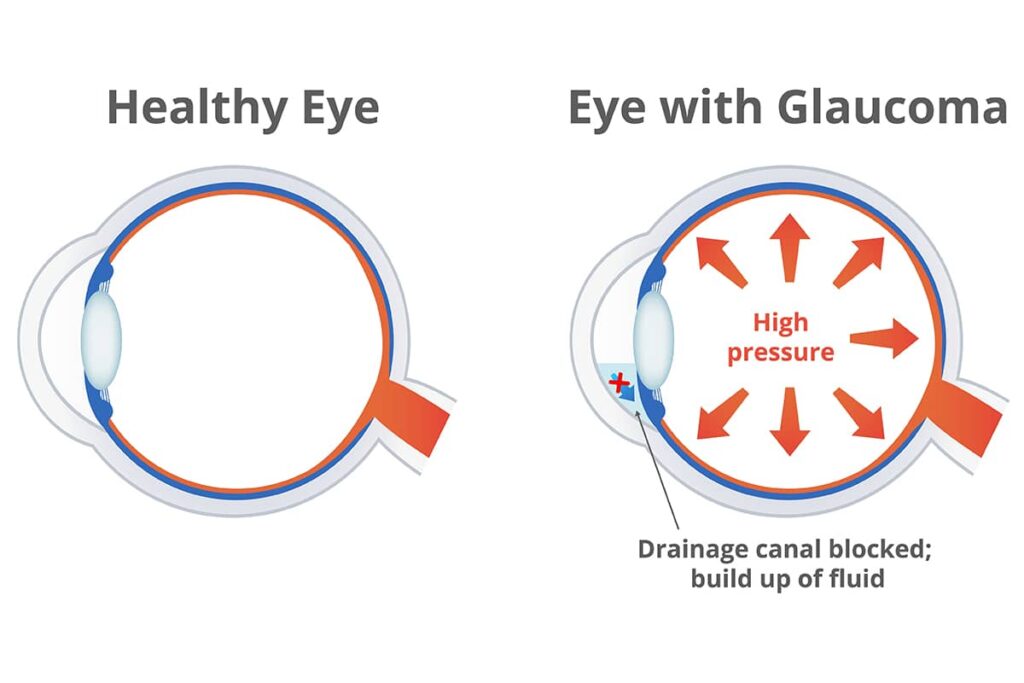
Glaucoma occurs when fluid builds up in the eye, increasing pressure within the eyeball that damages delicate tissues. While there are multiple causes of glaucoma, research has shown that people living with diabetes have an increased risk of developing this condition, as well as severe vision loss.
This article explores the link between diabetes and glaucoma, including what causes this link and how it can be managed. With the help of an experienced medical team and lifestyle changes, people living with both conditions may be able to reduce their risk of developing complications.
Diabetes is a Risk Factor for Glaucoma
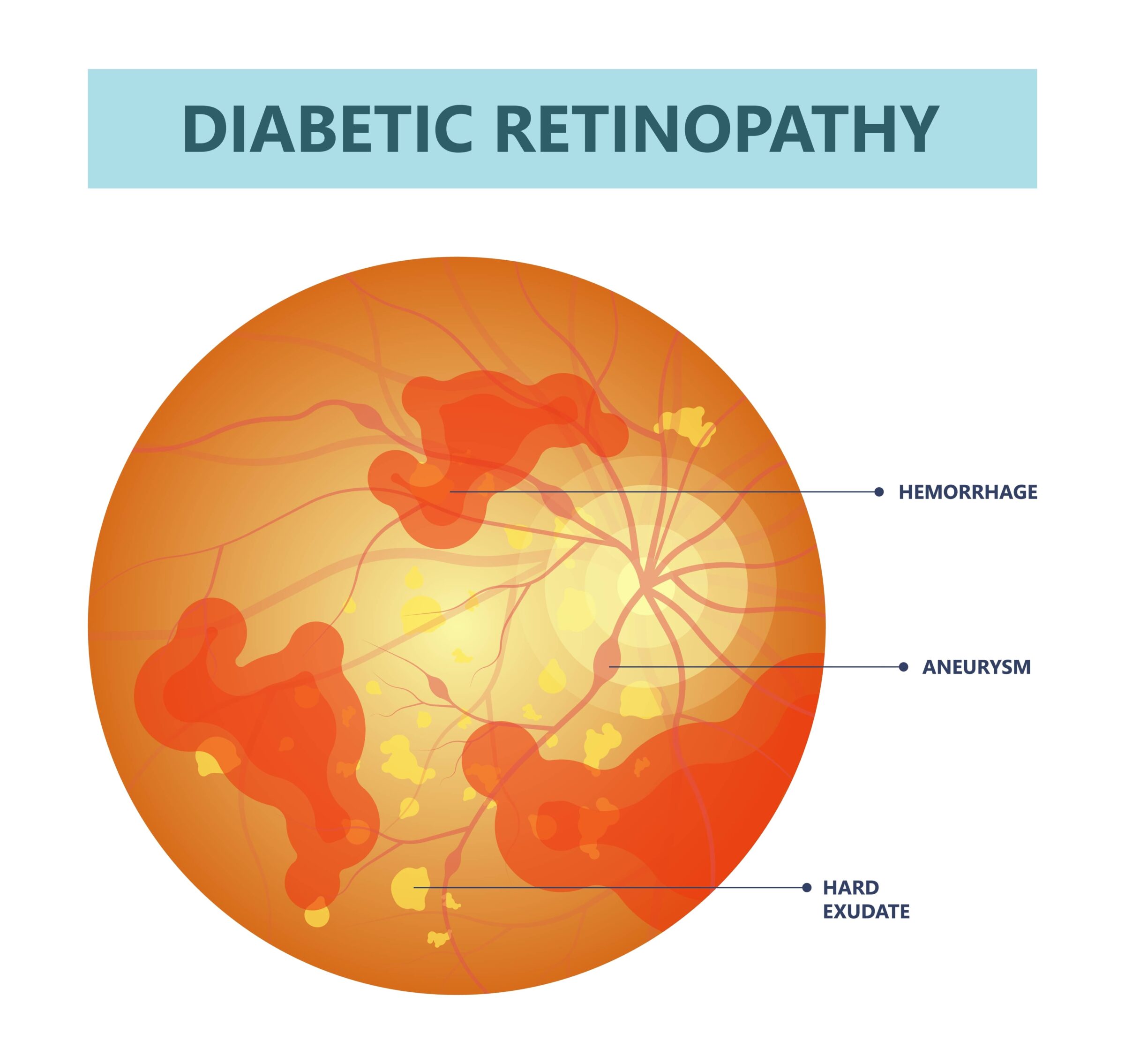
Individuals with a diagnosis of diabetes should be aware that they have a higher risk of glaucoma than people without diabetes. Diabetic retinopathy is a common form of diabetic eye disease that affects people with diabetes and can cause damage to the blood vessels in the retina. This damage can lead to increased pressure within the eyeball, which is one of the main causes of glaucoma. Additionally, high blood pressure associated with diabetes can also increase the risk of glaucoma.
Regular eye exams are essential for monitoring any changes in vision or warning signs of glaucoma. Additionally, blood sugar control and managing blood pressure help reduce the risk of developing this eye disease. With adequate management and lifestyle changes, people living with both conditions may be able to reduce their risk of complications from glaucoma.
Symptoms of Glaucoma in Diabetics
- Blurry vision: One of the primary symptoms of glaucoma in diabetics is hazy or blurred vision; people may lose a portion of their peripheral vision or have difficulty seeing things that are far away.
- Puffy/swollen eyes: Diabetics with glaucoma may experience eye puffiness and swelling due to an increase in intraocular pressure (IOP). This can result in a noticeable increase in “eye bags.”
- Seeing halos around lights: Halos, glowing circles, or rainbows appearing around bright objects can be a symptom of ocular hypertension, which is one of the conditions associated with glaucoma.
- Headaches and pain in the eyes: Glaucoma is known to cause headaches and irritating pain in the eyes when severity increases. The eyes may also start to feel itchy, dry, red, and/or sore at times.
- Nausea: Another symptom caused by glaucoma that is common in diabetic patients is nausea. This sensation can range from feeling slightly queasy to having more intense experiences.
- Eye floaters: Eye floaters appear when dots or other shapes drift across the field of vision. This symptom can be very dangerous for those suffering from glaucoma, as it could indicate irreversible nerve damage has occurred.
- Loss of visual acuity: Visual acuity is a measure of how sharp images appear to you on an eye chart. If this level decreases, then it usually means that some type of complication has occurred, such as glaucoma-induced optic foraminal narrowing or retinal damage from chronically high intraocular pressure (IOP) levels caused by diabetes-related vascular disease.
- Difficulty adjusting to darkness: People with glaucoma and diabetes may find it takes longer for their vision to adjust to the darkness.
- Double vision: Diabetics with glaucoma may experience double vision, or seeing two images instead of one. This can be a sign of nerve damage caused by increased pressure in the eye.
- Loss of color perception: Glaucoma can cause a loss of color perception, making it difficult for people with diabetes to distinguish between colors.
- Tunnel vision: Tunnel vision occurs when people are only able to see what is directly in front of them and have difficulty seeing objects on the sides or periphery.
- Eye fatigue: Eye fatigue occurs when people feel tired after looking at something for too long or have difficulty focusing their eyes on an object for an extended period of time.
- Sensitivity to light: People with glaucoma and diabetes may also experience sensitivity to light, which can make it difficult for them to be outside during the day or to look at screens.
What Treatments Are Available for Glaucoma Caused by Diabetes?
Here are some treatment options for glaucoma caused by diabetes:
1. Ocular Hypertension Treatment (OHT)
Also known as topical ophthalmic glaucoma treatments, these can be used to lower ocular hypertension. This hypertension is essentially an increase in intraocular pressure (IOP) caused by either an imbalance in the production and drainage of aqueous humor or increased resistance at the blood–eye barrier.
The main goal of these treatments is to reduce IOP without adversely causing distortion of vision while reducing possible side effects associated with the long-term use of medical therapy.
2. Eye Surgeries
Eye surgeries are a common treatment option for glaucoma caused by diabetes. These procedures can be used to reduce IOP and improve vision. The most common treatment is a laser treatment known as trabeculoplasty, which uses a laser to open up the drainage channels in the eye, allowing fluid to flow more freely and reducing IOP.
Other forms of glaucoma surgery include filtration surgery, which creates a new pathway for fluid to drain from the eye, and tube shunt surgery, which involves implanting a tiny tube into the eye that helps regulate fluid levels. All of these surgeries have proven effective in treating glaucoma caused by diabetes, but they do come with some risks, such as infection or bleeding. Patients have to ask their doctor if they are candidates for glaucoma surgery before deciding on any type of surgical procedure.
3. Monitoring/Medication Combination
Your doctor may decide to treat your diabetes-related glaucoma with medications and aggressive monitoring. Surgical intervention may not always be necessary; it could depend on how severe the eye condition is and its progression rate over time.
Usually, low doses of medications are given first before stronger doses are prescribed if the low dose fails to prevent further damage.
4. Macular Edema Therapy
Macular edema can occur when fluid accumulates around the macula due to certain disorders, such as diabetes and central retinal vein occlusion (CRVO). Treatments for this involve using intravitreal injections of anti-VEGF drugs directly into the eye to help reduce fluid buildup and improve vision function.
5. Hyperosmotic Agents
Hyperosmotic agents are a type of medication used to treat glaucoma caused by diabetes. These medications work by drawing fluid out of the eye and reducing intraocular pressure (IOP). They can be taken orally or applied directly to the eye as an eyedrop. Common hyperosmotic agents include glycerin, mannitol, and urea.
These medications are generally well tolerated and have few side effects, but they may cause temporary blurred vision or stinging in the eyes. Hyperosmotic agents can help reduce IOP and prevent further damage to the optic nerve.
6. Nutrition Therapy
Eating a well-balanced diet rich in vitamins C & E, lutein, and zinc can preserve your eye health by protecting the eyes from oxidative damage caused by free radicals or elements like lead or selenium that cause cell death or disruption in tissue containing photoreceptors (rods and cones). This is particularly important for those who suffer from forms of diabetic retinopathy.
7. Diabetic Monitoring & Maintenance
A major component of treating glaucoma related to diabetes is monitoring glucose levels throughout all stages. This requires blood tests and annual eye exams. In addition, keep track of food intake, such as carbohydrates, fats, and proteins, on a daily basis by maintaining an individualized meal plan tailored to your needs.
Early Detection is Key to Treating and Managing Glaucoma in Diabetics
Early detection is key to treating and managing glaucoma in diabetics. It is important for those with diabetes to be aware of the types of glaucoma that can occur due to their condition, as well as the signs and symptoms associated with it. Glaucoma can be caused by an increase in eye pressure, which can be a result of poor blood flow or high average blood sugar levels. Therefore, it is essential for those with diabetes to have annual dilated eye exams to detect any changes in their vision or the presence of glaucoma. During these annual exams, the doctor will check for signs such as optic nerve damage, visual field loss, and other indicators that may suggest a history of glaucoma.
Once glaucoma has been detected, a treatment plan should be developed based on the individual’s needs. This plan may include medications such as eye drops or oral medications that help reduce eye pressure and improve blood circulation around the eyes. Additionally, lifestyle modifications, such as eating a healthy diet rich in vitamins C and E, lutein, and zinc, can help protect against oxidative damage caused by free radicals or elements like lead or selenium that cause cell death or disruption in tissue containing photoreceptors (rods and cones).
Finally, regular monitoring of glucose levels and maintaining a personalized meal plan can help keep diabetes in check and reduce the risk of developing glaucoma.

Ready for a consultation?
If you are looking for treatment options and want state-of-the-art glaucoma treatment, you will need a doctor with experience. The eye specialists at EyeSight Hawaii in Honolulu, HI, and Maui, HI have the knowledge to help. Make an appointment online or call our office to schedule a consultation today!